Lung diseases continue to claim millions of lives globally, presenting a major public health issue that demands urgent attention. Despite the advancement in medical science, treatment options are still quite limited, leaving patients with chronic conditions like chronic obstructive pulmonary disease (COPD) and cystic fibrosis in dire need of better alternatives. The conventional reliance on animal models for research and development of treatments has proven increasingly inadequate. Nonetheless, a pioneering study reported in *ACS Applied Bio Materials* has made significant strides in creating a mucus-based bioink aimed at 3D printing lung tissue, offering new hope for researchers and patients alike.
Many individuals grappling with severe lung diseases find themselves in a precarious situation. While organ transplants can provide a lifeline, the availability of donor organs remains critically low, causing an urgent need for innovative solutions. Most patients are relegated to treatment regimens that focus solely on symptom management due to the absence of cures. This systemic problem highlights a critical gap in the medical field that necessitates urgent research for more effective medications.
The current norm includes using animal models, particularly rodents, to assess the efficacy of potential drugs. However, these models often fall short in replicating the complexities of human lung physiology. Consequently, results derived from such studies may not offer a reliable foundation for understanding how new treatments could function in human patients. This inconsistency illustrates the pressing need for alternatives that can more accurately simulate human pulmonary conditions.
In light of the limitations associated with traditional treatment and research methodologies, bioengineering presents an intriguing frontier. By harnessing the power of 3D printing, researchers have begun exploring the potential of creating lab-grown lung tissue. This innovative approach not only aims to provide a more authentic model for studying lung diseases but also holds promise for future implant materials that could replace damaged tissue.
The main challenge faced by scientists in this endeavor has been the formulation of a bioink that can effectively support cell growth while maintaining its structural integrity. The breakthrough made by Ashok Raichur and his research team serves as a beacon of hope in this ongoing quest. Their use of mucin—a mucus component previously underutilized in bioprinting—has opened new avenues for lung tissue bioengineering.
The Breakthrough: Mucin-Based Bioink
Raichur and his colleagues embarked on a novel journey by transforming mucin into methacrylated mucin (MuMA), a compound that possesses certain molecular structures akin to epidermal growth factor, a protein essential for cell attachment and proliferation. By integrating lung cells with this bioink, the researchers addressed a crucial barrier in the development of functional lung tissue.
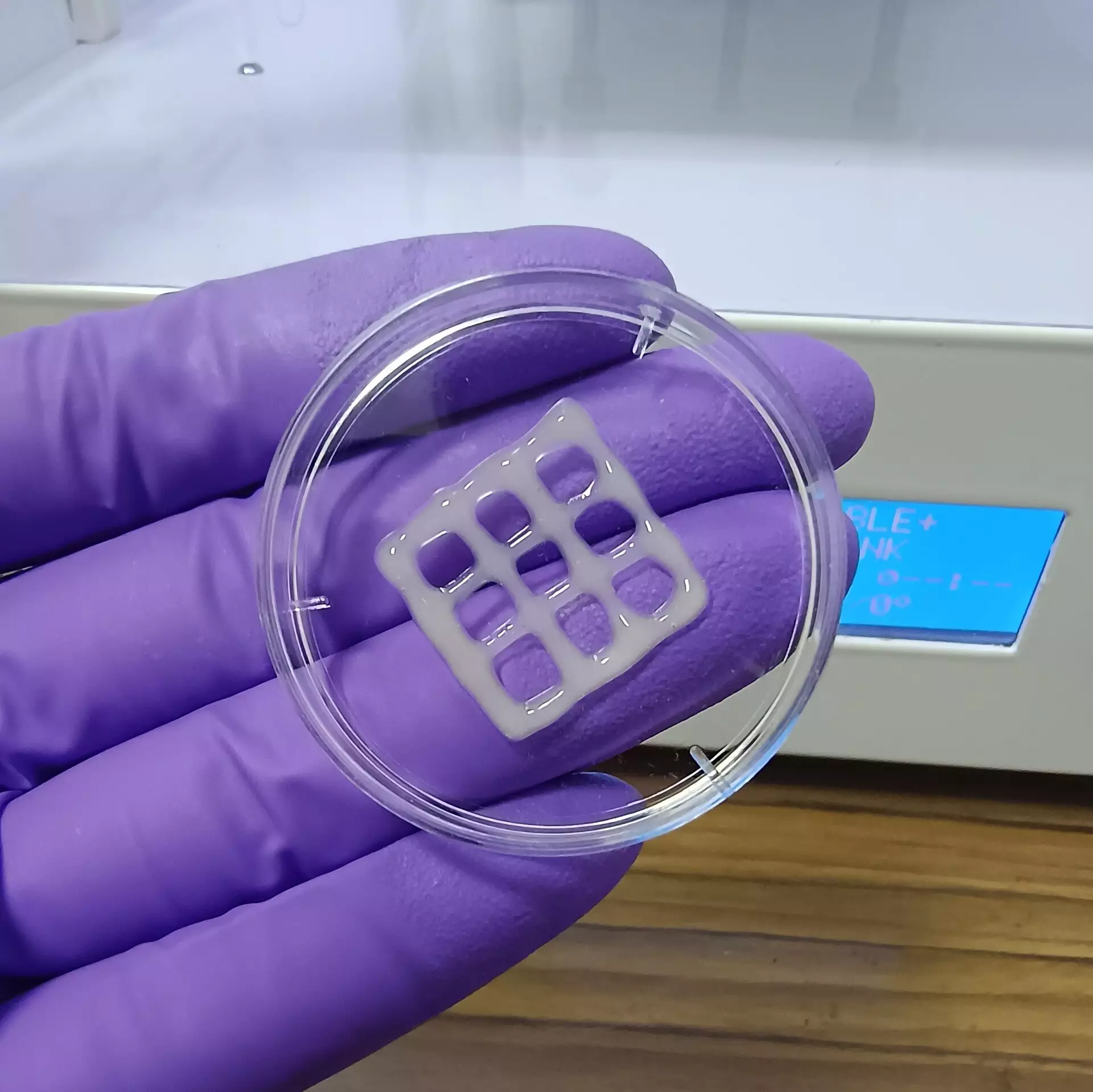
To enhance the viscosity and promote better cell adhesion, hyaluronic acid—a naturally occurring polymer—was added to the mix. Once the bioink was printed into various configurations, it underwent a process of crosslinking through exposure to blue light. This pivotal step resulted in the formation of a porous gel structure capable of absorbing moisture, thus fostering an environment conducive for cell survival.
The interconnected architecture of the gel demonstrated vital capabilities, including a swift diffusion of essential nutrients and oxygen, critical factors that encourage cell growth and healthy lung tissue formation. Moreover, preliminary tests indicated that the structures created were non-toxic and exhibited a slow biodegradation rate, suggesting their potential in clinical applications where they could eventually be replaced by organic lung tissue.
Future Implications and Applications
The ramifications of this groundbreaking research are monumental, suggesting that these mucus-based bioinks might not only revolutionize the study of lung diseases but could also be instrumental in the development of next-generation treatment modalities. The potential to create 3D models of lung tissue allows scientists to better investigate and understand the pathophysiology of various pulmonary disorders, thereby facilitating the evaluation and optimization of new treatments.
As research progresses, the hope is that bioengineered lung tissue could transition from laboratory settings to real-world clinical applications, offering potential solutions for patients suffering from chronic lung conditions. Overall, the invention of mucus-based bioink represents a significant leap forward in medical science, providing a robust framework for advancing lung disease research and treatment innovations. The intersection of bioengineering and medicine promises an exciting horizon for improving patient outcomes in the battle against lung diseases.

Leave a Reply