The effects of hormones on the physical body are widely recognized, especially in female reproductive health. However, a groundbreaking study from neuroscientists at the University of California, Santa Barbara unveils that these hormonal fluctuations also extend far beyond the uterus, profoundly influencing the very structure of the brain itself. This research led by Elizabeth Rizor and Viktoriya Babenko meticulously trails the nuances of hormonal impacts throughout different stages of the menstrual cycle, inviting us to reconsider what we know about women’s health and brain science.
Exploring the Cycle: A Closer Look at Structural Changes
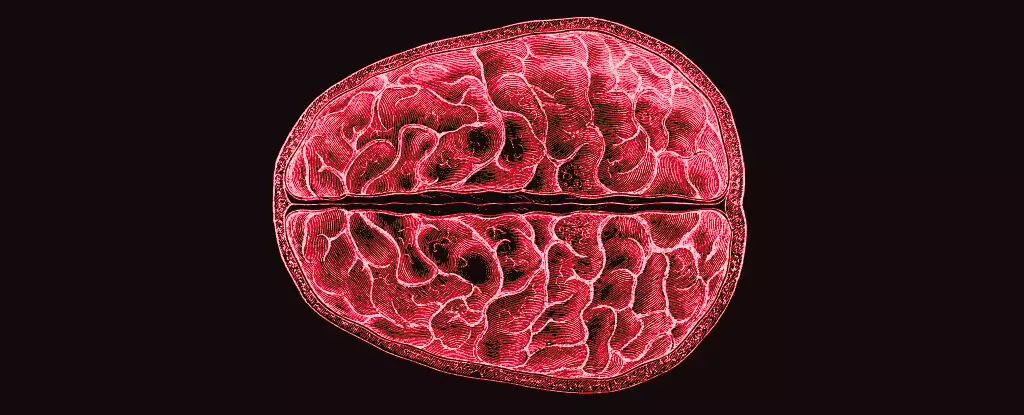
For decades, the conversation around menstrual health has been overshadowed by stigma and ignorance, leaving a gap in scientific inquiry. Rizor and Babenko’s team took a bold step to fill this void by closely examining 30 women’s neurological changes at various stages of their menstrual cycles: during menses, ovulation, and the mid-luteal phase. Their detailed MRI scans not only highlighted the brain’s response to fluctuating hormone levels but also illustrated changes in white matter microstructure and cortical thickness. This insightful approach was groundbreaking, asserting that changes are not confined to traditionally studied areas like the hypothalamic-pituitary-gonadal (HPG) axis but can pervade the brain at large.
Their findings illustrate variations in gray and white matter volumes alongside cerebrospinal fluid dynamics, suggesting that hormonal shifts can lead to profound structural changes. For example, heightened levels of 17β-estradiol and luteinizing hormone prior to ovulation correspond with a notable twitch in white matter integrity, signaling potentially enhanced communication processes across brain regions. This not only sheds light on the cyclical nature of feminine health but poses complex questions about the interplay between hormonal balances and cognitive functions.
Breaking Ground on Women’s Health Research
One cannot overlook the startling reality that menstrual health research has historically lagged behind studies focusing on male biological dynamics. It’s a glaring disparity in a field intensely affecting half the global population for a significant portion of their lives. “Why haven’t we explored this sooner?” is the crucial inquiry that emerges. Rizor, Babenko, and their team’s inquiry, however, does much more than fill a research gap; it emphasizes the critical need for a paradigm shift in scientific exploration.
By concentrating on brain structural changes rather than merely cognitive tasks, the researchers push the boundaries of traditional neuroscience. Their findings reveal hormonal fluctuations affect the central nervous system in ways that demand our attention and deserve more elaborate study. When cyclic variations in hormones like progesterone and follicle-stimulating hormone are linked to substantial changes in brain structure, it raises important discussions about women’s mental health, behavioral patterns, and how they may correlate with the passing of their menstrual cycles.
The Implications for Mental Health
Moreover, the research invites contemplation about the connection between these structural changes and the mental health challenges that many women face, particularly those related to menstruation. The relationship between fluctuating hormones and mental state is well acknowledged, yet empirical grounding around the structural impact on the brain is remarkably scarce. Given the potential links between white matter changes and cognitive behaviors, it opens doors to understanding women’s experiences of mood disorders, irritability, and period-related mental health issues.
The results indicate a strong relationship between hormone-driven phenomena and brain microstructure, with implications that might well inform therapeutic approaches or clinical practices. As society increasingly recognizes the importance of mental health, can we now afford to ignore the role of hormonal cycles in shaping women’s psychological well-being? Each cycle, with its myriad of effects, could potentially hold clues to ameliorating severe mental health issues associated with the menstrual cycle.
These key revelations from the UCSB research represent not just an academic win; they herald a new era in understanding women’s health, fostering a culture where complex interactions between hormones and brain structures are seen as worthy of exploration and intervention.

Leave a Reply