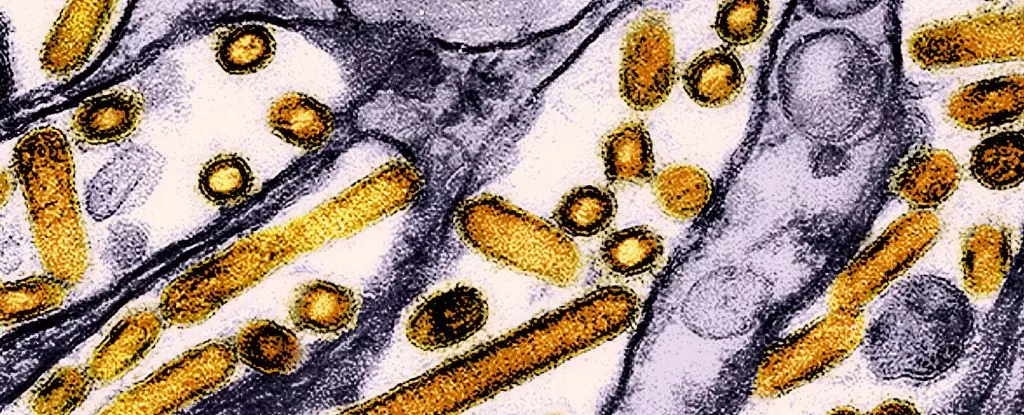
The emergence of new infectious diseases has been a significant public health concern over the last few decades. One such disease making headlines is the highly pathogenic avian influenza (HPAI), particularly the H5N1 strain, known for its severe impact on bird populations and potential risk to human health. Recent studies from Michigan and Colorado have shed light on the presence of H5N1 antibodies in dairy workers, suggesting an unnoticed transmission of this virus to humans through occupational exposure. Here, we will explore the implications of these findings and their broader relevance to public health.
A study conducted by the Centers for Disease Control and Prevention (CDC) examined blood samples from 115 dairy workers, revealing that 7% of them had antibodies indicative of previous infection with the highly virulent H5N1 virus. This statistic is alarming, yet it also brings forth a silver lining: most of those infected exhibited mild symptoms or none at all. Notably, many reported ailments such as sore throats, fevers, or eye irritation but did not require hospitalization. This suggests a potential asymptomatic carriage, which complicates our understanding of the virus’s transmission dynamics.
Despite the relatively low severity seen in these dairy workers, the implications of allowing this virus to circulate undetected raise fundamental concerns. The existence of such antibodies prompts an urgent need for monitoring, especially as unchecked viral spread increases the chances of mutations that could heighten the virus’s virulence and transmissibility.
Recent outbreaks in other countries serve as grim reminders of how quickly the situation can escalate. A hybrid strain of the H5N1 virus recently appeared in Cambodia, resulting in three fatalities. Genetic studies indicate this new variant may possess mutations that enhance its capacity for airborne transmission and pose a threat to mammals, including humans. Such developments underline the importance of global surveillance systems in tracking infectious diseases and provide a cautionary tale about the need for robust response mechanisms.
The recent case from Canada, involving a teenager suffering from a mutated strain believed to be associated with the US outbreak in dairy cows, reflects similar concerns. This individual’s condition highlights the evolving risk factors that human populations may face as these viruses continue to adapt. So far, this appears to be an isolated incident, yet it reflects the ever-present risks that viral mutations pose to public health.
The connection between farmworkers and the potential introduction of avian influenza into the human population cannot be overlooked. All the dairy workers in the mentioned study were engaged in close contact with cattle, with none reportedly following best practices for personal protective equipment (PPE). This negligence raises alarms about occupational safety in agricultural settings, where the risk of zoonotic diseases is compounded by proximity to infected animals.
CDC health scientists emphasize the need for targeted outreach and education, particularly for Spanish-speaking workers who may be more vulnerable due to cultural and language barriers. Effective interventions must encompass culturally sensitive communication strategies that inform agricultural workers about infection prevention measures, including the proper use of PPE.
The rising incidence of HPAI in the US dairy sector, with over 400 infected herds across 48 states, makes it imperative to enhance infectious disease monitoring and management strategies. The dire consequences witnessed since 2022, including the culling of over 90 million domestic birds in the US, indicate a necessary shift in public health policies globally.
Authorities advocate for robust hygiene practices around animals and encourage reporting unusual occurrences of sick or dead wildlife. Understanding symptoms of the disease in animals, such as lethargy or difficulty in mobility, is equally crucial for early detection.
Furthermore, initiatives like the vaccination program for California condors exemplify proactive steps taken to mitigate the effects of HPAI on endangered species. Simultaneously, research is underway to develop a human vaccine against H5N1, emphasizing a multi-faceted approach to addressing this looming public health crisis.
The findings related to avian influenza in humans emphasize the need for heightened awareness of zoonotic diseases, improved safety practices in agricultural environments, and collaborative global efforts to monitor and manage outbreaks. If left unchecked, the mutations and spread of HPAI could not only pose great risks to agricultural economies but also threaten global health security.

Leave a Reply