Recent advancements in neuroscience have unveiled a potentially transformative drug designed to combat inflammation in the brain, which has been found to enhance the integrity of the blood-brain barrier in animal models. Researchers led by pathologist Sanford Markowitz at Case Western Reserve University (CWRU) have made significant strides in understanding the role of a specific immune protein, 15-PGDH, in neurodegenerative diseases such as Alzheimer’s. This discovery is particularly thrilling given the chronic challenge faced by current Alzheimer’s treatments, which predominantly focus on the removal of amyloid proteins with limited success. By recognizing a new pathway for intervention, researchers are exploring a promising avenue that could open doors to more effective treatments.
Understanding the Blood-Brain Barrier’s Role
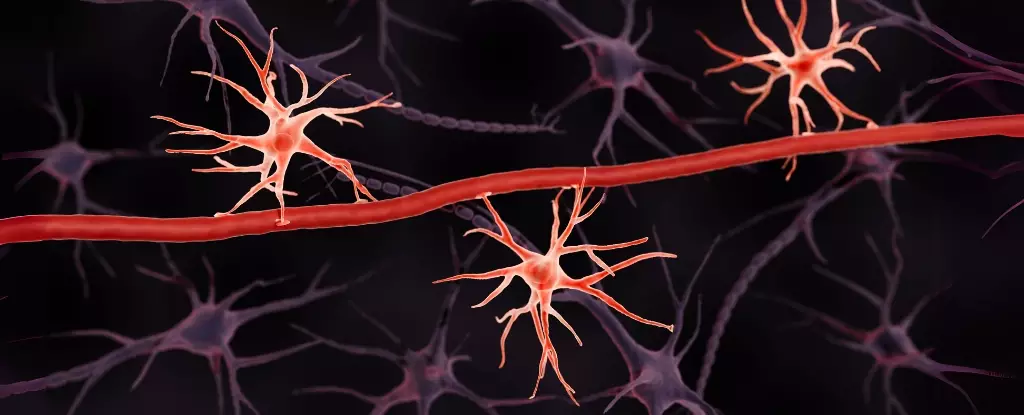
The blood-brain barrier serves as a highly selective shield that prevents harmful substances from penetrating brain tissue. Maintaining its integrity is crucial, as its deterioration has been linked to early signs of dementia and neurodegeneration. This novel approach targeting inflammation presents a paradigm shift. Damage to the blood-brain barrier increases vulnerability to various neurotoxins, emphasizing the need for protective therapies. The insights gained by researchers at CWRU, especially regarding the enzyme 15-PGDH, illuminate the complex interactions between inflammation and neurodegenerative disease processes. By developing the compound SW033291 to inhibit this enzyme, the research team successfully upheld the barrier’s protective function in mouse models.
A Breakthrough in Existing Treatment Paradigms
What’s groundbreaking about this new therapy is its distinct mechanism. Unlike conventional Alzheimer’s medications, which largely aim to clear amyloid deposits yet often bring about adverse effects, this drug offers a fresh perspective. Researchers have noted that despite maintaining amyloid levels, the new treatment proves effective in preserving cognitive function and preventing neurodegeneration following traumatic brain injuries. The implications of such a finding could redefine treatment strategies, ushering in a new era for individuals facing cognitive decline.
It is crucial to highlight the gravity of dementia’s rising prevalence, with an estimated 10 million new cases globally each year. Traditional treatment avenues have yielded insufficient results, accentuating the urgent need for innovative strategies. The identification of 15-PGDH as a guardian of the blood-brain barrier not only demonstrates a novel approach but also offers hope in the relentless pursuit of effective therapies for neurodegenerative conditions.
The Road Ahead: Competition and Hope
As promising as these findings are, it is essential to recognize that there remains a long journey ahead. Navigating the complexities of translating these results from animal models to human application will require extensive clinical trials and rigorous testing to ensure safety and efficacy. While optimism is warranted, it must be tempered with realism regarding the challenges associated with developing new medications. Each advancement in understanding the brain’s intricate mechanisms can pave the way for groundbreaking therapies that could ultimately improve countless lives affected by cognitive decline.
This research underscores the vital intersections of inflammation, neurodegenerative disease, and the blood-brain barrier, yielding potential therapeutic breakthroughs that go beyond the limitations of current treatment paradigms. The future looks promising for a brain health revolution, one where targeted therapies could gain the upper hand against debilitating cognitive diseases.

Leave a Reply